We hope that your experience in recent hospital admission and Intrathecal Baclofen pump implant has been smooth and positive and you are already experiencing the benefit of the ITB pump.
This booklet has been written by the Spasticity Team at the National Hospital for Neurology and Neurosurgery.
It is intended for patients (or anyone who is involved in their care) who have undergone implantation of an Intrathecal Baclofen Pump under the care of the team at this hospital. It is not intended to replace discussion with your treating team.
If you have any questions, please do not hesitate to contact a member of our team, we will be happy to answer them for you.
Spasticity can be described as involuntary muscle stiffness often associated with spasms, pain, weakness and clonus. Once exercises, physiotherapy and oral medications are tried and proven ineffective, ITB (Intrathecal Baclofen) treatment is considered to manage spasticity. Following a successful ITB trial, implantation of an ITB pump is completed. ITB pump system delivers baclofen directly into the cerebrospinal fluid (CSF) filled space surrounding the spinal cord (intrathecal space) where concentration of the nerve receptors sensitive to baclofen are found.
The pump system consists of a pump and catheter (Figure1). The pump is placed under the skin in the abdomen and a catheter connects the baclofen-filled reservoir to CSF in the intrathecal space around the spinal cord (Figure 2). The catheter is tunneled from the lower lumbar spine around the waist to the abdomen so that the complete system remains hidden under the skin. The pump is made of titanium and looks like a round metal disk 8.75cm (3.4 inches) in diameter and 2.6cm (1.0 inch) in thickness. The pump battery lasts 81 months and you will be admitted for pump replacement before the battery runs out.
Figure 1: Pump
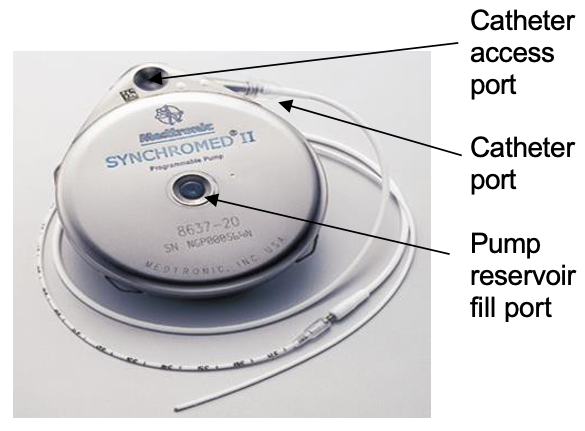
Figure 2: Positioning of pump and catheter

It is extremely important to remain as active as possible once your ITB pump is fitted. Regular stretches, active and passive movements of your limbs should continue daily where possible. There are however a few adaptations that we would recommend following implantation of an ITB pump.
Below is intended to act as a guide to you and those assisting you to move after ITB pump implantation, and has been designed from questions asked by our current ITB users. The majority of patients have their ITB pump implanted in their abdomen and the advice and recommendations we provide here focusses on this pump location site.
You will be advised on any specific adaptations to exercises, activities of daily living and transfers that we would recommend you follow if you have the pump implanted in an alternative site.
As with any surgery the time of most risk is immediately after the surgery and in the first six to eight weeks. This is due to the fact that the wounds need time to heal.
Are there any movements I should adapt?
Try to adapt your position to avoid bending forward past 90 degrees in sitting or standing. Try and move your body or chair closer to the object or use ‘easy-reach’ equipment to assist you.




Try to avoid leaning excessively backwards when exercising.

To move up the bed, try where possible to push through your legs in a bent position with your arms by your side rather than pulling yourself with your arms above your head. If you have a hospital profiling bed, use the movement of the bed to reposition yourself.
To reduce excessive twisting of your back, bring things to your side to access rather than twisting around. If you can move your wheelchair to avoid twisting and sustained rotations, this is preferable to minimise risk.


Do I have to adapt my transfers when I have an ITB pump?
The safest method for your transfers will be established in hospital prior to your discharge home and will be reassessed when you come in for your first physiotherapy review and then at your annual ITB physiotherapy review.
Whether you transfer using a banana board, pivot or standing, please avoid any direct pressure over the pump and intrathecal catheter site (around waist) as this can damage the integrity of the pump system. We do not recommend the use of manual handling belts around your waist or toilet hoist sling for the same reason.
Full body hoist: there is very minimal risk to the intrathecal catheter or the ITB pump when using a full body hoist.
Lifting: we do not recommend that you are manually lifted for any transfers. Lifting is a physical strain for those who lift you and can also damage the intrathecal catheter.
Can I use standing equipment, such as a motorised standing frame?
We recommend you wait until your six-week physiotherapy review before commencing or resuming use of motorised standing equipment. This allows time for the surgical wounds to heal and a tailored re-assessment of the support needed to help you stand safely.
Standing hoist/Sara Steady/Cricket: please ensure the strap or standing hoist sling is supporting you around your bottom/pelvis, and not on your pump or catheter site as this can damage the intrathecal catheter when moved into standing. Some equipment may be compatible for use with a pelvic strap instead of a waist strap so please discuss this with your therapist or the NHNN Spasticity Team.

Rota stand/ Re-turn: if another person is helping you to stand, ensure that they support you around your pelvis, and not “pulling you up” under the arms or waist.
We are happy to work with your local therapists to discuss concerns that you may have with your standing equipment at home and provide recommendations to ensure you maximise the benefit that the ITB system gives you. It is important that you or others do not alter any piece of equipment, ensuring you always use equipment within the manufacturer’s guidelines.
Can I lie on my pump?
We recommend that you do not lie directly on your pump site.
If you sleep on your front, we would advise you to use soft pillows or cushions to minimise the pressure on the pump and catheter.
Do I have to adapt any of my exercises?
We suggest that when stretching your lower limbs and back that your legs are not brought up together into a flexed position towards your chest – either by you or someone else. You can bring one leg up at a time to stretch and move. Stretches to the lower back in which you lie with your knees bent and then rotate your legs to the side into a corkscrew position are also best avoided. Remember this for personal care tasks completed on the bed.


When lying on your front do not come up into the cobra position as this will narrow the vertebral spaces within the spine and may damage the intrathecal catheter.

You can still engage in activities such as exercise classes safely by adapting the range of the exercises you do and not combining bending with twisting.
Abdominal exercises: we recommend that you do not perform traditional “sit up” exercises. If you would like to train your abdominals we would suggest you do static contractions, pelvic floor contractions, “bridging” or work in sitting if you are able.
Gym equipment: we recommend you seek specific guidance from your spasticity physiotherapist and a personal trainer. When exercising, it is very important to be aware of your posture and be in supported postures whilst training. Many of our patients’ complete weight training but we do recommend you seek advice before commencing such a programme.
Vibration plates (Vibrogym) are NOT safe to use with an ITB pump in place – please see manufacturer’s manual for further details.
Swimming/Hydrotherapy: you can swim and complete exercises within the water with an ITB pump implanted once your wounds have completely healed (usually after the physio review at six weeks post operation). We recommend you avoid excessive twisting of the back if others are stretching you in the water.
Extreme heat or high/low pressure can affect the pump i.e., hot sauna, sunbathe, flight, scuba dive, hyperbaric oxygen therapy. Please refer to the pump manual which was given to you after the operation or seek further advice from the team for more detailed advice if you are planning any of these activities.
FES can be used but we would recommend you do NOT use it directly over the abdomen. Please see individualised advice at the end of this leaflet.
Advice from ITB pump users regarding adapting activities of daily living to avoid restricted movements:
- A helping hand or “grabber” can assist being able to pick objects up from the floor and avoid leaning excessively forwards, backwards or to the side.
- Putting your feet on a stool or raised surface to put socks and shoes on, avoids excessive bending of the trunk.
- Using small bean bag rolls or rolled up towels under a fitted sheet on your bed can help you remain in an adapted side lying position and not put pressure directly on the pump.
- Try and avoid tight fitting clothing that finishes directly on the pump site. Choose clothing that finishes above or below the pump site.
- You can adapt positions for sexual intercourse. Please feel free to discuss this with one of the members of the team.
Don’t let the ITB pump stop you moving or discourage others helping you to move and keep as active as possible. The correct movements and stretches are key to assisting managing your spasticity and keeping you comfortable. ITB catheter complications and pump malfunctions are rare but avoiding the positions and movements discussed above will reduce the risk of problems arising.
Going back to work
There are no clear rules on how long you should be off work after the pump implant. It really depends on the type of work you do and how quickly you recover from the operation. Generally, we advise to be off work until the surgical clips or sutures are removed and your wounds have healed completely which is usually seven to 14 days.
Driving
Driving is not restricted with ITB pump however, it is your responsibility to report to DVLA of your condition and organise an assessment for fitness to drive. We would advise you to avoid placing seat belt right over the pump site.
The main complication of the implantable pump system is that something goes wrong with the catheter; it is dislodged from the spine or becomes kinked, disconnected or torn. If this happens a further operation is required to replace the catheter.
The pump very rarely goes wrong or breaks down. If either the pump stops working or the catheter gets damaged the main risk is baclofen withdrawal. If the pump delivers too much baclofen or there is a prescribing error you can present with signs of baclofen overdose. The common effects of baclofen withdrawal and overdose are listed below.
If you experience these you should contact the team for further advice and you will need to attend hospital to have the pump investigated or dose adjusted.
Symptoms of baclofen withdrawal:
- Increase in stiffness or spasms Itching or goosebumps.
- Fast heart rate.
- Low blood pressure.
- Fever.
- Confusion or hallucinations Seizures.
- Agitation.
- Symptoms of baclofen withdrawal.
- Increase in stiffness or spasms Itching or goosebumps.
- Fast heart rate.
- Low blood pressure.
- Fever.
- Confusion or hallucinations Seizures.
- Agitation.
The three most common features of baclofen overdose:
- Drowsiness.
- Weakness of lower limbs.
- Dizziness/ light-headedness.
There are certain triggers (listed below) which can make your spasms or stiffness worse despite a working ITB pump system. It is important that you are aware of these and manage them appropriately. Prevention and early management are always advisable.
Trigger Factors:
- Urinary retention or infections Bowel impaction, constipation Poor positions in lying or sitting Low mood or stress.
- Pain.
- Red or broken skin areas Infections.
ITB pump may not resolve your pre-existing pain especially if this was not related to the spasticity and you may need to continue your pain medications. Please discuss with the team if you have concerns about any types of pain you experience after the pump implant and you may be referred to the pain specialist if necessary
You will have two wounds after the operation one on your abdomen and one on your lower back. Usually sutures or clips will be removed by a district nurse within 10 days of the operation however your wounds will continue to heal after the removal of sutures or clips. If there are any signs of wound infection such as redness, tenderness, swelling, leakage, temperature or skin breakdown, we advise you to contact your district nurse and spasticity team immediately.
The ITB pump is MRI conditional however it is important that you inform the MRI requester of the pump. We may take an x-ray of your abdomen beforehand to ensure your pump is sitting oblique and not in line with the bore magnet. The pump motor stalls during the MRI and it restarts by itself when you come out of MRI. This can take from 30 minutes to 24 hours. It is important your pump is checked after MRI to ensure that it has restarted.
Please inform the spasticity team as soon as your MRI is scheduled whether at the National Hospital for Neurology and Neurosurgery or elsewhere.
Your ITB pump may set off the metal detector at airports, so please present your identification card to the security personnel.
We advise you to check before travelling abroad that you have enough baclofen in the pump to cover your time away. In case of emergency, it is advisable that you identify the nearest ITB pump service to your holiday destination. We can assist you finding this.
After implantation of an ITB pump, you will be followed up regularly by our team as listed below. It is important you make an effort to attend all these appointments.
Four weeks: Nurse-led telephone clinic (no need to come to hospital)
Four to six weeks: Physio-led clinic in the gym
Six monthly: ITB pump refill in the Day Care Unit
Yearly: Physio-led clinic in the gym
We strongly advise you to continue to see your neurologist for ongoing management of your condition as ITB pump will not affect the progress of the condition you have.
Your GP will receive information on intrathecal baclofen and the contact procedures. The nurse specialist is available to offer advice and education to your community and social care team as needed. The nurse specialist is available Monday to Friday during office hours, out of hours advice is available through the doctor on call here or the nurse in charge of the ward you were admitted to.
If you wish to discuss any aspects further, please don’t hesitate to contact us.
The Spasticity Management Team
National Hospital for Neurology and Neurosurgery Queen Square
London WC1N 3BG
Admin queries: 0203 448 3112
Email: uclh.
Spasticity helpline Tel: 0203 448 3439
If not available please leave a message on the answer phone / voicemail and your call will be returned as soon as possible. The line is confidential.
Website: https://www.uclh.nhs.uk/spasticity-management
OUT OF HOURS EMERGENCY:
Please contact the hospital switch board on 0203 4567890.
Explain that you have an Intrathecal Baclofen Pump and request to be put through to the NEUROLOGY ON CALL REGISTRAR.
MS Society National Helpline:
MS Research Trust:
www.
The Neurological Alliance:
Medtronic website:
British Brain and Spine Foundation Helpline:
Scope:
http://
The Continence Foundation Helpline:
